The Role of Transradial Access Devices in Minimally Invasive Medicine
Transradial access devices (TRA) have become a preferred technique for catheter-based vascular interventions, providing a safer and more efficient alternative to transfemoral access (TFA). Initially introduced in cardiology, TRA is now widely used in neurovascular procedures, peripheral artery disease (PAD) treatments, and other endovascular interventions due to its lower risk of complications. Additionally, TRA offers faster patient recovery and improved procedural efficiency.
Unlike femoral access, which requires a larger puncture site in the groin, TRA allows physicians to introduce catheters and guidewires via the radial artery in the wrist. This minimizes bleeding complications, reduces hospital stays, and enables many procedures to be performed in an outpatient setting.
Understanding Transradial Access Devices
TRA devices are temporary-use instruments designed for short-term arterial access. These include:
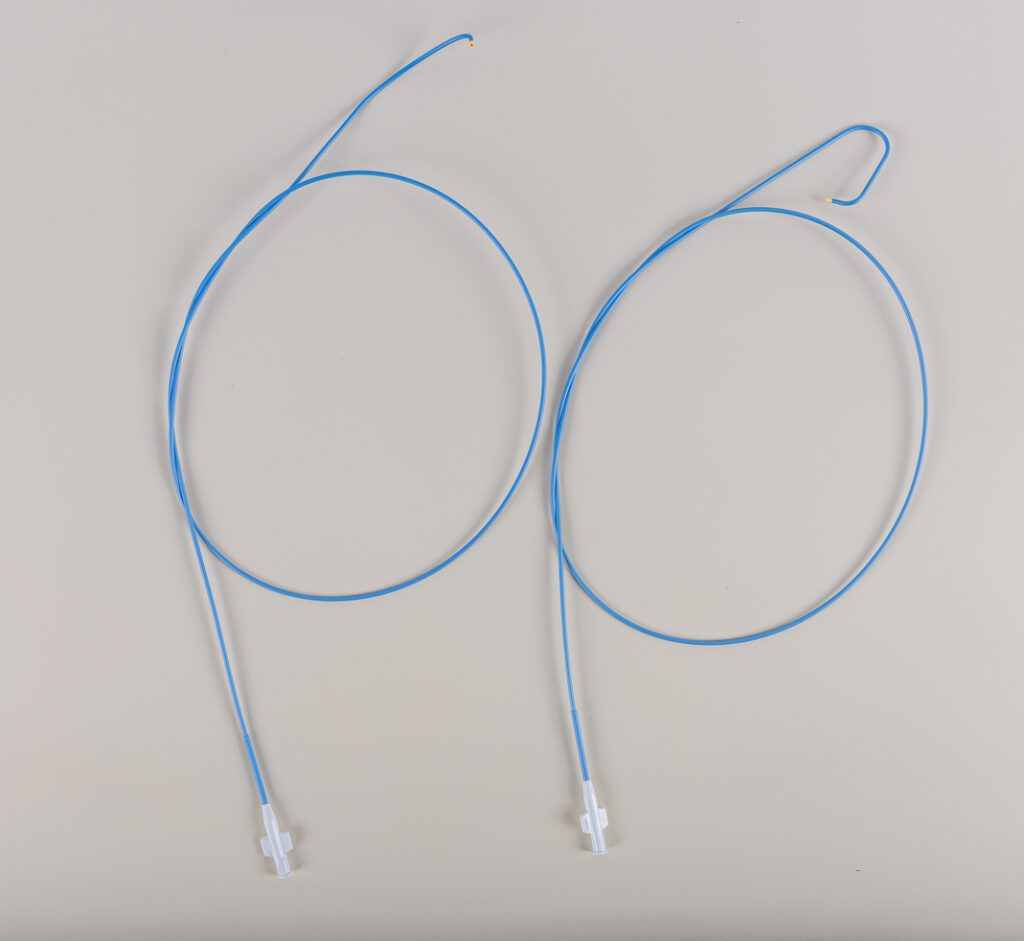
- Sheaths – Introduced into the radial artery to enable catheter insertion.
- Guidewires – Assist in navigating the vascular system safely.
- Catheters – Used for angiography, stent placement, and thrombectomy.
- Hemostasis Devices – Compression bands or wristbands that control bleeding post-procedure
Unlike permanently implanted devices such as stents or vascular grafts, TRA devices do not require endothelialization, as they are removed immediately after the procedure. Instead, their surfaces must be engineered for short-term blood compatibility, ensuring they are non-thrombogenic and non-irritating to the vessel walls.
Why Transradial Access is Gaining Widespread Adoption
TRA is now a standard approach for various procedures, including coronary angiography, percutaneous coronary interventions (PCI), neurovascular interventions such as mechanical thrombectomy for stroke, electrophysiology procedures, and peripheral artery disease (PAD) treatments. Several key advantages drive the widespread preference for TRA:
TRA is now a standard approach for various procedures, including coronary angiography, percutaneous coronary interventions (PCI), neurovascular interventions such as mechanical thrombectomy for stroke, electrophysiology procedures, and peripheral artery disease (PAD) treatments. Several key advantages drive the widespread preference for TRA:
It is associated with a significantly lower risk of major bleeding complications, as the radial artery is smaller and more superficial than the femoral artery, reducing vascular injury risks.
Patients undergoing TRA also experience faster recovery times, as they can sit up, move, and even be discharged sooner compared to femoral access, which often requires extended bed rest. This translates to greater patient comfort and satisfaction, particularly in outpatient procedures.
From an economic perspective, TRA leads to lower healthcare costs, as the need for intensive post-procedure monitoring is significantly reduced. These benefits have positioned TRA as the preferred access method for many interventional procedures, with increasing adoption across multiple medical specialties.
Challenges in Transradial Access Device Performance
Despite its advantages, TRA is not without challenges. The small size and unique anatomy of the radial artery introduce potential complications, particularly when device surfaces are not optimized for hemocompatibility.
Key Challenges Include:
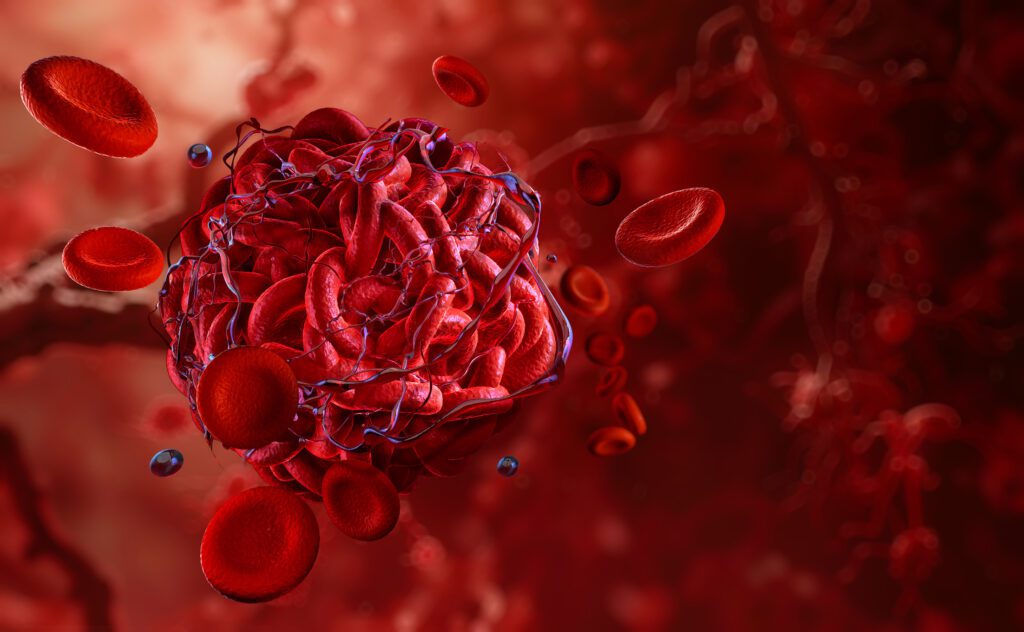
Thrombogenicity – Contact with artificial surfaces may activate platelets, leading to clot formation and vascular obstruction.
Radial Artery Spasm (RAS) – A sudden narrowing of the artery can hinder catheter manipulation and prolong procedural time.
Surface Friction & Vessel Trauma – If a device lacks sufficient lubricity, it may cause irritation, discomfort, or microtrauma to the arterial walls.
To mitigate these risks, advanced surface coatings are required to improve the safety and effectiveness of TRA devices.
To mitigate these risks, advanced surface coatings are required to improve the safety and effectiveness of TRA devices.
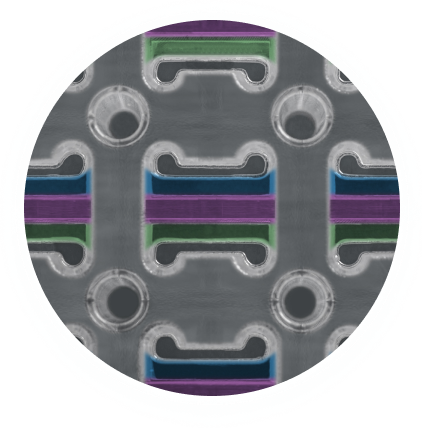
The Role of Camouflage™ Coating in Optimizing Transradial Access Devices
At Smart Reactors, we develop biocompatible coatings that enhance the functionality and safety of medical devices. Our Camouflage™ coating technology is specifically designed to optimize TRA sheaths, guidewires, and catheters, addressing key clinical concerns:
- Hemocompatibility Enhancement – Camouflage™ minimizes platelet adhesion and clot formation, reducing the risk of thrombosis.
- Anti-Spasm Properties – A low-friction surface reduces irritation, lowering the risk of radial artery spasm.
- Enhanced Lubricity – Improves catheter navigation, ensuring smooth insertion and removal with minimal arterial trauma.
- Durability & Biocompatibility – Designed for short-term blood compatibility, ensuring optimal performance throughout the procedure.
By incorporating Camouflage™ coating, medical device manufacturers can enhance the reliability, safety, and efficiency of TRA devices, ultimately improving patient outcomes.
Advancing Transradial Access Through Surface Innovation
As the medical industry shifts toward minimally invasive procedures, the demand for high-performance vascular access devices continues to grow. While TRA offers significant advantages over femoral access, the success of each procedure depends on the quality and biocompatibility of the devices used.
By integrating advanced hemocompatible coatings, Smart Reactors is at the forefront of medical device innovation. We provide next-generation surface modification solutions that reduce procedural risks, enhance operator control and precision, and improve patient safety and experience.
- Reduce procedural risks
- Enhance operator control and precision
- Improve patient safety and experience
For device manufacturers looking to optimize their transradial access technology, Camouflage™ offers a proven solution.
To learn more about how Smart Reactors’ Camouflage™ coating can enhance your transradial access devices, contact us today.
Share this post: on LinkedIn