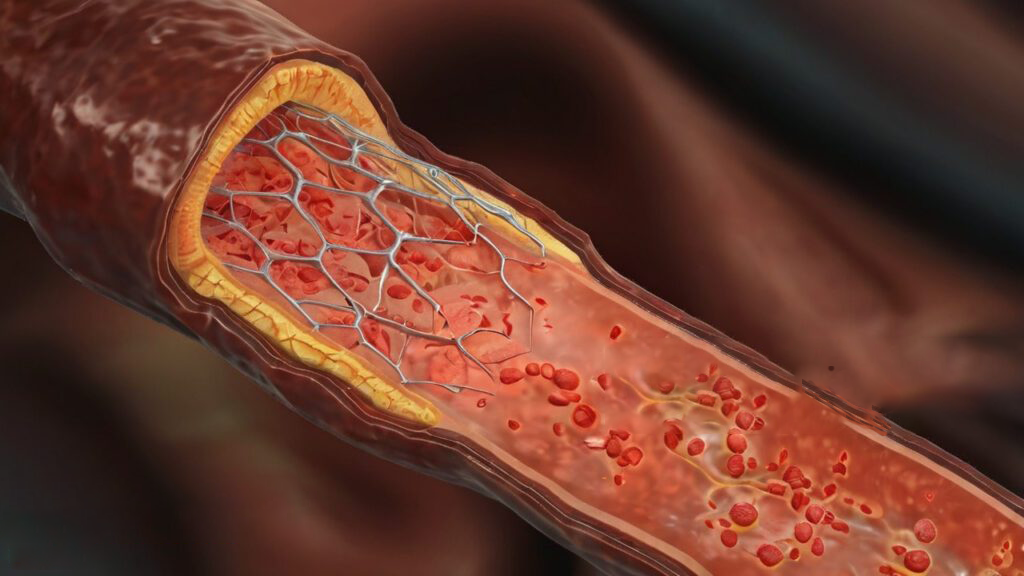
Flow diverters have brought significant advancements in treating complex intracranial aneurysms, providing a minimally invasive solution to redirect blood flow and promote vessel healing. However, as with many endovascular devices, maintaining long-term efficacy requires overcoming the challenge of restenosis—a condition where excessive tissue growth narrows the treated vessel over time. Preventing restenosis is essential to sustaining the success of flow diverters, and anti-restenotic coatings have emerged as a powerful tool to tackle this challenge.
This article explores how these innovative coatings work to maintain vessel patency, improve patient outcomes, and extend the effectiveness of flow diverters in neurovascular treatments.
The Mechanisms Behind Restenosis

Restenosis is driven by the body’s response to foreign objects, often resulting in an overgrowth of cells around the implanted device. This condition is largely attributed to:
- Neointimal Hyperplasia: A rapid buildup of smooth muscle cells that accumulate within the vessel wall and narrow the lumen.
- Inflammatory Reactions: Chronic inflammation around the device site can promote excessive tissue growth, obstructing blood flow.
- Extracellular Matrix Buildup: Proteins and other extracellular materials deposit in the vessel, further narrowing the lumen.
Mr Brian Haddigan, co-founder of Smart Reactors, emphasizes, “Restenosis is the Achilles’ heel of many endovascular treatments. By focusing on prevention through advanced coatings, we’re aiming to significantly improve long-term outcomes for patients.”
The Role of Specialized Coatings in Restenosis Treatment
Anti-restenotic coatings provide flow diverters with a protective layer that directly addresses the triggers for restenosis, reducing cell proliferation, modulating inflammation, and encouraging healthy vessel integration. These coatings are tailored to support the specific needs of neurovascular applications, helping to prevent tissue buildup and maintaining vessel patency over time. Effective anti-restenotic coatings serve several critical functions:
- Inhibit Smooth Muscle Cell Growth: Anti-proliferative agents are designed to prevent the rapid cell growth that contributes to lumen narrowing.
- Reduce Inflammation: By minimizing inflammatory reactions, coatings support a stable environment, limiting tissue overgrowth.
- Promote Controlled Endothelialization: Coatings that encourage endothelial cell attachment and growth help create a smooth, protective lining, which prevents restenosis by reducing unwanted cell migration.
Innovative Coating Technologies to Prevent Restenosis
Today’s anti-restenotic coatings offer diverse approaches to tackling the challenges of restenosis. From drug-eluting formulations to bioresorbable layers, these coatings provide solutions that adapt to the body’s healing processes, reducing risks associated with untreated flow diverters.
| Types | What they are | What they do |
|---|---|---|
| Polymer-Free Coatings | For patients who may be sensitive to polymers, polymer-free coatings provide an alternative that reduces inflammation risk. Utilizing nanoporous surfaces or direct drug-binding, these coatings: | Lower the inflammatory response associated with polymer degradation. Promote faster endothelialization, with complete vessel coverage achievable within about 28 days. Improve overall biocompatibility, enhancing long-term safety by minimizing foreign material presence. |
| Drug-Eluting Coatings | Drug-eluting coatings are one of the most effective methods for directly combating restenosis. These coatings deliver precise, localized doses of anti-proliferative drugs like sirolimus, paclitaxel, or everolimus, which act on smooth muscle cells to reduce neointimal hyperplasia. Key benefits include: | A controlled drug release that prevents excessive cell growth at the device site. Sustained release profiles extending up to 90 days, are essential for early-stage restenosis prevention. Reduced systemic side effects, as the drugs are concentrated locally rather than throughout the body. |
| Nitric Oxide (NO)-Releasing Coatings | NO-releasing coatings deliver nitric oxide, a natural molecule that inhibits smooth muscle cell proliferation and reduces thrombosis risk. These coatings enhance flow diverter outcomes by: | Inhibiting smooth muscle growth by up to 50%, helping to maintain vessel patency. Promoting endothelial cell health, creating a natural, anti-thrombotic environment. Reducing platelet adhesion, potentially minimizing the need for extended antiplatelet therapy. |
| Bioresorbable Coatings | Bioresorbable coatings are designed to deliver anti-restenotic benefits during the critical healing phase and gradually dissolve, leaving behind a bare metal surface. This strategy is beneficial because it: | Provides targeted restenosis prevention in the initial 3-6 months post-implantation. Reduces the long-term presence of foreign material, lowering chronic inflammation risks. Allows flexibility for combining with other treatments for a phased, multi-targeted approach. |
| Biomimetic Phosphorylcholine Coatings | Designed to mimic the surface of red blood cells, phosphorylcholine coatings improve blood compatibility and lower inflammation. These coatings prevent restenosis by: | Reducing protein adsorption that can trigger immune responses. Decreasing inflammatory cell adhesion, ensuring a stable, smooth healing process. Enhancing hemocompatibility reduces clot formation around the device. |
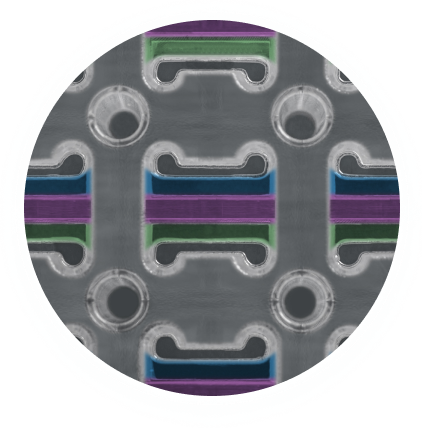
| Nanostructured Surface Coatings | Nanostructured coatings offer a biomimetic approach by creating surfaces that encourage healthy tissue integration. These coatings: | Facilitate endothelial cell adhesion, reducing restenosis risk by encouraging a natural healing response. Control protein interactions to modulate cellular activity and support balanced healing. Provide a nanoscale structure that mimics natural tissue, further enhancing device compatibility. |
Mark Brassil, Co-Founder of Smart Reactors, states, “Our Camouflage™ coating combines multiple mechanisms to create a synergistic effect, addressing the complex biological processes that lead to restenosis.”
Clinical Impact of Anti-Restenotic Coatings
The adoption of anti-restenotic coatings in flow diverters has led to significant improvements in clinical outcomes. Recent studies show that coated devices can reduce restenosis rates by up to 60% at the one-year mark, with patency rates remaining high at 90% or more over two years. These results indicate a substantial reduction in the need for reinterventions, providing potential cost savings of $10,000-$15,000 per patient due to fewer follow-up procedures. Additionally, anti-restenotic coatings may enable shorter durations of dual antiplatelet therapy (DAPT), reducing it from the standard 6-12 months to as little as three months in some cases.
This reduction is particularly valuable for patients at high bleeding risk or those with upcoming surgical procedures, making treatment safer and more accessible. Looking forward, developments in combination coatings could enhance clinical outcomes even further. These coatings integrate multiple agents to deliver synergistic effects—such as combining sirolimus with NO-releasing compounds for both anti-proliferative and healing benefits. Emerging smart coatings, capable of responding to biological cues, as well as nanotechnology-enhanced surfaces that provide precise and sustained drug release, represent promising directions for the future.
Advancing Neurovascular Care with Anti-Restenotic Coatings
Specialized coatings for preventing restenosis represent a transformative advancement in neurovascular treatments, addressing the critical challenge of vessel re-narrowing and enhancing patient outcomes. By preventing tissue overgrowth and supporting a stable healing process, these coatings significantly expand the long-term efficacy of flow diverters and reduce the need for reinterventions.
At Smart Reactors, we are dedicated to pioneering coating technologies with our proprietary Camouflage™ coating. This multi-functional coating addresses both immediate and prolonged restenosis risks, offering a comprehensive solution tailored to the complex demands of neurovascular treatments. As innovations continue, the future of flow diverters looks bright, with coatings that enable safer, more effective, and longer-lasting results for patients worldwide.
Share this post: on LinkedIn