Cardiovascular devices, such as stents, heart valves, vascular grafts, and pacemakers, are critical for managing a wide range of circulatory system conditions. While these devices are engineered for durability and functionality, their performance and success heavily depend on their ability to integrate seamlessly with the human body. Coatings designed specifically for cardiovascular devices have emerged as essential tools in addressing challenges like thrombosis, inflammation, and biofouling, while enhancing biocompatibility and long-term performance.
Why Coatings Are Essential for Cardiovascular Devices
The interface between cardiovascular devices and blood presents unique challenges due to the dynamic nature of the circulatory system. These include:
- Thrombosis Prevention:
- Uncoated devices often trigger platelet activation and thrombus formation, which can block blood flow and lead to life-threatening complications. The ability of coatings to minimize platelet adhesion and fibrin deposition is crucial for maintaining device patency and ensuring safety.
- Reduction of Inflammatory Responses:
- Foreign materials can provoke immune reactions, causing inflammation and fibrosis that compromise device function. Coatings that improve the electrochemical surface properties, such as the implantation of negative ions, have demonstrated significant potential in reducing inflammation and promoting healing.
- Endothelialization Support:
- Many devices require a coating to promote the growth of a natural endothelial layer, reducing thrombogenicity and enhancing integration. Enhancing the adhesiveness of biomaterial surfaces with specific molecules, such as fibronectin or integrin-binding peptides, can significantly improve endothelial cell retention under dynamic flow conditions.
- Durability Under Dynamic Stress:
- Coatings protect devices from mechanical wear and degradation due to constant blood flow and pressure fluctuations, ensuring the longevity of implants in high-stress environments.
- Biofouling Mitigation:
- Coatings help prevent the accumulation of proteins, cells, and bacteria, which can impede device performance and lead to infections.
Endothelialization: A Critical Component of Cardiovascular Device Biocompatibility
Endothelialization is fundamental to ensuring the long-term success of cardiovascular implants. This process involves the formation of a stable endothelial layer on blood-contacting surfaces, mimicking the natural lining of blood vessels. To achieve this, various strategies have been developed, ranging from modifying surface properties to delivering growth factors that stimulate endothelial cell (EC) proliferation and migration.
One effective approach is the use of porous biomaterials and coatings that enable spontaneous endothelial ingrowth. These materials promote angiogenesis, allowing endothelial cells to migrate and populate the surface. Additionally, the surface functionalization of biomaterials with peptides, such as RGD sequences, has been shown to significantly enhance EC adhesion and proliferation, even under high-shear conditions.
Advanced coatings go further by enabling the delivery of pro-angiogenic growth factors or leveraging autologous ECs or stem cells to improve cellular retention. Techniques that increase cell adhesion through specific covalent linkages or tailored electrochemical properties are increasingly being integrated into next-generation cardiovascular devices.
Applications of Coatings in Cardiovascular Devices
Device Type | Purpose | Coating Needs |
| Stents | Maintain vessel patency in cases of arterial blockage. | – Anti-thrombogenicity to prevent blood clots. – Endothelialization support for rapid healing. |
| Heart Valves | Replace or repair damaged valves, ensuring unidirectional blood flow. | – Hemocompatibility to reduce clot formation. – Wear resistance to withstand continuous movement. |
| Vascular Grafts | Bypass or replace damaged vessels. | – Hemocompatibility for thrombus prevention. – Support for tissue integration and endothelialization. |
| Pacemakers and ICDs | Regulate or restore heart rhythm. | – Antimicrobial properties to prevent infections. – Biocompatibility to reduce fibrotic encapsulation. |
| Catheters and Extracorporeal Circuits | Facilitate blood flow or procedures outside the body. | – Hemocompatibility to reduce thrombus formation. – Lubricity for ease of insertion and reduced trauma. |
Smart Reactors’ Camouflage™ Coating: Revolutionizing Cardiovascular Devices
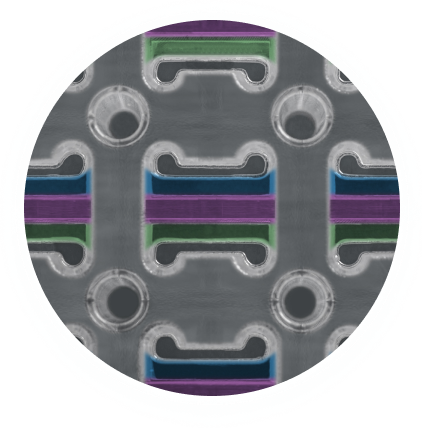
Smart Reactors’ Camouflage™ coating represents a breakthrough in addressing the challenges faced by blood-contacting implants. Designed with advanced biomaterial science, Camouflage™ enhances biocompatibility by creating a non-thrombogenic surface that reduces platelet adhesion and activation. This feature minimizes the risk of thrombus formation, a critical requirement for cardiovascular devices operating in high-stress environments.
A standout feature of Camouflage™ is its ability to support natural endothelialization without relying on pharmacological agents. The coating promotes endothelial cell adhesion and proliferation, fostering the growth of a stable and biocompatible endothelial layer. Additionally, its durable design ensures that the coating maintains structural integrity under the dynamic blood flow conditions typical of cardiovascular implants. By leveraging micro- and nano-texturing techniques, Camouflage™ enhances cellular interactions, further improving its performance as a next-generation solution.
Unlike drug-eluting coatings, which carry potential side effects, Camouflage™ relies on its inert and biomimetic properties to deliver exceptional biocompatibility. This innovation aligns with the industry’s growing emphasis on safer, long-lasting, and more effective implant solutions.
Clinical Impact of Cardiovascular Device Coatings
The evolution of specialized coatings has transformed the functionality and clinical success of cardiovascular devices. Enhanced endothelialization through advanced coatings like Camouflage™ has led to significant improvements in patient outcomes, reducing complications such as thrombosis and restenosis. These advancements have also extended the lifespan of implants by ensuring better integration and reducing the need for revision surgeries.
Coatings now enable cardiovascular devices to function in increasingly complex clinical scenarios, from intricate small-diameter stents to large-scale vascular grafts. By focusing on biocompatible and non-drug-eluting solutions, the industry is moving toward safer and more sustainable designs that prioritize patient well-being and long-term performance.
Share this post: on LinkedIn